PCOS
A misunderstood disease
Polycystic Ovarian Syndrome (PCOS) is one of the most misunderstood and mistreated disease states in medicine.
PCOS- a subgroup disorder
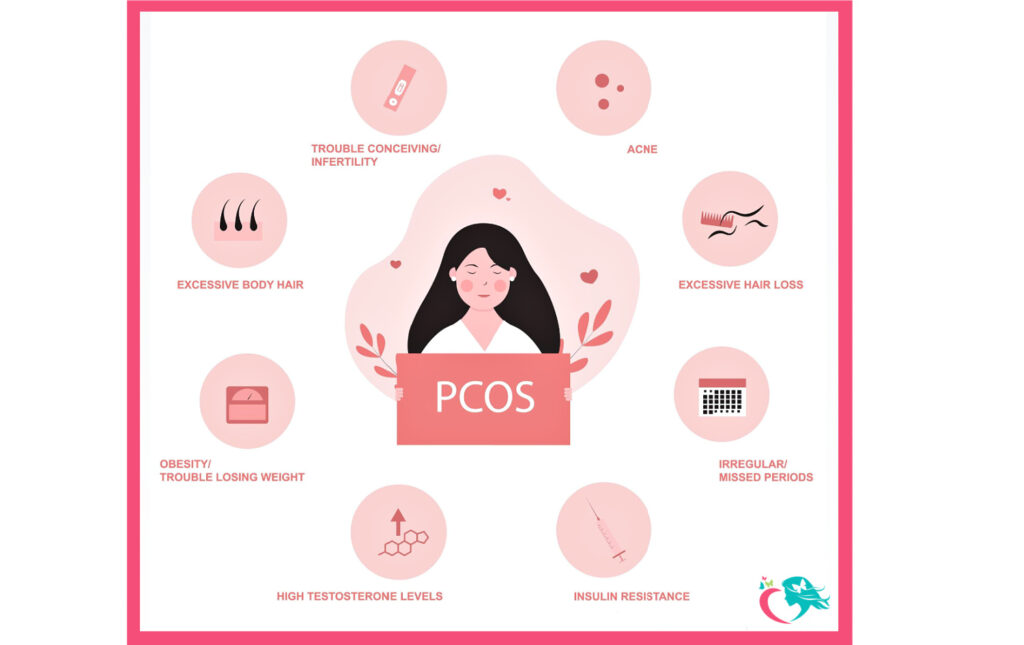
PCOS is actually part of a much larger group of hormonal disorders in women that result in the overproduction of testosterone (the main male hormone). Every woman produces some testosterone, but at much lower levels than men. When a woman’s testosterone levels are higher than that of a normal woman (known as an androgen excesses) one commonly experiences one or more side effects that include:
- Oily skin
- Acne
- Hair growth on the face and abdomen (hirsutism)
- Irregular and occasionally heavy menses
- Infertility or sub-fertility, including early miscarriages
Overactive glands in Testosterone production
Women produce testosterone in the ovaries and the adrenal glands. If one or both of these glands becomes overactive in testosterone production, then the woman will experience the typical effects of testosterone listed above.
The overproduction of androgens
In PCOS the source of the overproduction of testosterone is the ovaries. While there are several mechanisms that can cause the ovaries to overproduce testosterone, PCOS is one of the most common. PCOS occurs due to an imbalance in the pituitary hormones FSH (follicle stimulating hormone) and LH (leutinizing hormone). These two pituitary hormones stimulate ovarian ovulatory activity and hormone production.
Different types of cells in the ovary
There are several different types of cells in the ovary. Some of the cells (theca cells and interstitial cells) produce testosterone when stimulated by LH or insulin.
Other ovarian cells (granulosa cells), stimulated by FSH, absorb the testosterone that is produced and convert it to estrogen under the influence of the enzyme aromatase. This conversion of testosterone to estrogen in the ovary is a normal activity of the ovary and is how the ovary produces estrogen.
Levels of testosterone
High levels of testosterone in the ovary can occur if the LH or insulin levels are high. These high levels overwhelm and shut down the aromatase enzyme. This results in the blockage of testosterone conversion to estrogen and testosterone builds up in the ovary. This excess testosterone is eventually released into the bloodstream.
In PCOS, high levels of testosterone in the bloodstream are converted to high levels of estrogen in the bloodstream. High blood levels of estrogen then cause the pituitary gland (a small gland at the base of the brain) to release of high levels of the hormone LH into the blood stream. High levels of LH in the blood stream then stimulates the ovary to produce more testosterone. This creates a “vicious cycle” that fosters continued high testosterone levels and results in all of the adverse effects of high testosterone blood levels previously described.
High levels of estrogen
High levels of estrogen at the pituitary gland also cause the FSH levels to be low. This low FSH causes the ovary to be less effective in converting testosterone to estrogen. This combination of the high LH and low FSH also results in uneven stimulation to the ovaries and the loss of ovulation in the ovaries.
This ovulatory dysfunction of the ovaries also causes the developing eggs in the ovaries to stop their growth as 10-12 mm cysts. The eggs in these cysts can’t ovulate. These small cysts persist and build up in the ovary resulting in enlargement of the ovary. This causes the classic “polycystic” appearance of the ovary (and hence “polycystic ovarian disease”).
When ovaries do not ovulate, irregular periods, prolonged and heavy periods and infertility occur.
Insulin, along with LH, has the ability to directly stimulate the ovaries to produce testosterone. High levels of insulin (insulin resistance) directly increase the production of ovarian testosterone resulting in the clinical picture described above.
Adrenal glands
High blood levels of testosterone can also occur when testosterone is overproduced by the adrenal glands. These high levels of testosterone can cause the ovaries to over produce testosterone
As you can see, while the clinical picture (acne, excess hair growth, irregular periods, difficulty conceiving) of these 2 conditions can look similar, the causes are frequently significantly different. The best treatment results are always achieved when the cause of the testosterone overproduction is identified and treated directly and correctly.
PCOS and all conditions causing an elevation of blood testosterone levels are best treated by a Reproductive Endocrinologist/Gynecologist like Dr. Burke who specializes in the treatment of women’s hormonal imbalances and is best qualified to help you achieve your goals.
Appointments
If you are struggling with PCOS, do not hesitate and call now to schedule an appointment to talk with Dr. Burke about your concerns.
Call us at 856-429-2212
Additional articles you might find helpful…